Why Therapists Aren’t Utilizing Biofeedback as Often as They Should
NeuroRehab Team
Wednesday, August 28th, 2024
Introduction
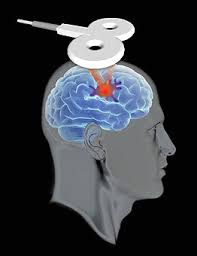
Biofeedback is a powerful therapeutic technique that provides patients with real-time information about their physiological processes, empowering them to actively monitor and regulate their own bodily functions. Yet, despite its proven benefits, biofeedback remains significantly underutilized in the therapy world. In this comprehensive article, we’ll explore the reasons behind this underutilization and uncover the compelling advantages that make biofeedback a must-have tool in every therapist’s arsenal.
The Mechanics of Biofeedback
At its core, biofeedback involves the use of specialized equipment to measure and display various physiological signals, such as muscle tension, brain activity, heart rate, and skin temperature. By providing patients with immediate, visual or auditory feedback on these internal processes, biofeedback enables them to consciously control and modify their bodily responses. This real-time information allows patients to gain a deeper understanding of their own physiological states and develop effective self-regulation strategies.
The Proven Benefits of Biofeedback
The research on the efficacy of biofeedback is extensive and compelling. Numerous studies have demonstrated its ability to:
- Improve Postural Control and Balance: Biofeedback can help patients with neurological conditions or physical impairments to enhance their postural stability and balance, reducing the risk of falls and improving overall mobility.
- Enhance Strength and Range of Motion: By providing feedback on muscle activity, biofeedback can guide patients in developing better muscle control, leading to increased strength and improved range of motion.
- Reduce Spasticity and Spasms: Biofeedback has been shown to be effective in managing spasticity and involuntary muscle spasms, a common challenge for individuals with neurological disorders.
- Minimize Compensatory Movements: By highlighting areas of weakness or overcompensation, biofeedback can help patients identify and correct unhealthy movement patterns, promoting more efficient and natural movement.
- Activate Force Couples: Biofeedback can be used to target and activate specific muscle groups that work together as “force couples,” improving overall motor control and coordination.
- Improve Motor Control: The real-time feedback provided by biofeedback allows patients to refine their motor skills, leading to enhanced control and precision in their movements.
- Break Up Synergies: Biofeedback can help patients overcome the challenge of “synergies,” where multiple muscles are activated together, by enabling them to isolate and control individual muscle groups.
These are just a few of the many benefits that make biofeedback a valuable tool for therapists working with a wide range of patient populations, from stroke survivors to individuals with musculoskeletal disorders.
The Underutilization of Biofeedback in Therapy
Despite the substantial evidence supporting the efficacy of biofeedback, it remains significantly underutilized in the therapy world. Several factors contribute to this phenomenon:
- Lack of Awareness: Many therapists may not be fully aware of the capabilities and applications of biofeedback, limiting its adoption within their practices.
- Perceived Complexity: The technical nature of biofeedback equipment and the need for specialized training can create a perception of complexity, deterring some therapists from incorporating it into their treatment approaches.
- Reimbursement Challenges: Depending on the healthcare system and insurance coverage, the costs associated with biofeedback equipment and specialized training may not be adequately reimbursed, making it a less appealing investment for some practitioners.
- Time Constraints: In today’s fast-paced healthcare environment, therapists may feel pressed for time, and the additional setup and patient education required for biofeedback may be seen as a barrier to its widespread implementation.
- Resistance to Change: Some therapists may be hesitant to adopt new technologies or techniques, preferring to stick to familiar methods, even if biofeedback could potentially offer superior outcomes for their patients.
Overcoming the Barriers to Biofeedback Adoption
To address the underutilization of biofeedback in the therapy world, several strategies can be employed:
- Increased Education and Awareness: Continuing education programs, professional development workshops, and industry publications can help therapists gain a deeper understanding of the benefits and applications of biofeedback, dispelling misconceptions and promoting its adoption.
- Streamlined Training and Implementation: Manufacturers and biofeedback experts should work to develop more user-friendly equipment and provide comprehensive training programs to ease the technical barriers for therapists.
- Advocacy for Reimbursement: Healthcare organizations and professional associations can advocate for improved reimbursement policies that recognize the value of biofeedback and make it a more financially viable option for therapists.
- Demonstrating Tangible Outcomes: By consistently documenting and sharing the positive outcomes achieved through biofeedback, therapists can build a compelling case for its widespread adoption, highlighting the tangible benefits for both patients and practitioners.
- Fostering a Culture of Innovation: Therapy practices should cultivate an environment that encourages the exploration and integration of new technologies, such as biofeedback, to stay at the forefront of evidence-based, patient-centered care.
The Future of Biofeedback in Therapy
As the healthcare landscape continues to evolve, the role of biofeedback in therapy is poised to grow. Advancements in technology, such as the integration of wearable sensors and mobile applications, are making biofeedback more accessible and user-friendly. Click here to see some of the latest advances in Biofeedback that is currently commercially available. Additionally, the increasing emphasis on personalized, data-driven healthcare is likely to drive greater adoption of biofeedback as a valuable tool for tailoring interventions and monitoring patient progress.
By embracing biofeedback and overcoming the barriers to its implementation, therapists can unlock a powerful set of capabilities that can transform the way they approach patient care. From enhancing physical rehabilitation to supporting mental health and wellness, biofeedback has the potential to revolutionize the therapy field, leading to better outcomes, improved patient engagement, and more efficient, holistic care.
Conclusion
Biofeedback is a powerful therapeutic technique that has been consistently shown to deliver significant benefits for patients across a wide range of conditions. Yet, its underutilization in the therapy world remains a puzzling reality. By addressing the factors that contribute to this underutilization and fostering a culture of innovation, therapists can unlock the full potential of biofeedback and elevate the standard of care they provide. As the healthcare landscape continues to evolve, the integration of biofeedback into therapy practices will become increasingly crucial, paving the way for more personalized, data-driven, and effective patient outcomes.
Free Neuro Balance CEU Course Now Available
NeuroRehab Team
Thursday, May 11th, 2023
Improving Dynamic Balance Following Neurological Injury
Overview:
This AOTA approved continuing education class will introduce you to efficacous evidence-based interventions that drive neuroplastic change resulting in improved balance following neurological injury.
The online class is intended for medical professionals (e.g. OT/OTA, PT/PTA, Physicians, etc.) directly related to the rehabilitation of a patient or client. To participate in this CEU and receive credit, the participant must be a licensed, treating clinician. Completion of this course will reward the participant with .1 CEUs or 1 contact hours, following completion of the presentation and a ≥ 80% score on the quiz. You will have 90 days to complete this course.
Stroke Hand Recovery CEU Course Now Available
NeuroRehab Team
Friday, March 10th, 2023
Stroke Hand Simplified
Evidence-Based Strategies to Help Restore, Rewire and Recover

Register Now
6 Tips to Build Trust with Stroke Patients
NeuroRehab Team
Friday, March 3rd, 2023
Suffering from a neurological injury such as stroke can be a long and hard battle. Having the right team in place can make a significant impact on the success of one’s recovery. Being comfortable with one’s clinical team can set patients up for great success. Health professional building that immediate trust is key to a positive outcome.
Stroke Therapy Research. What works?
NeuroRehab Team
Friday, January 13th, 2023
Arm and HandElectrical StimulationHand Function SplintsMental PracticeMirror TherapyNeuroplasticityStroke Statistics
Every 2.1 seconds, someone in the world suffers a stroke. Stroke is the #1 cause of long-term disability worldwide. Globally, there are over 15 million stroke survivors. With respect to the United States, there are approximately 5.1 million stroke survivors alive today in the US. It is the third leading cause of death in USA and the numbers are expected to double by 2030.
Free Constraint-Induced Movement Therapy CEU Course for OT’s
NeuroRehab Team
Wednesday, December 28th, 2022
Course Title:
Constraint-Induced Movement Therapy. Understanding the Facts and Myths.
Overview:
This AOTA approved online self-study continuing education class will introduce you to evidence-based practice surrounding Constraint-Induced Movement Therapy to the stroke population.
The online class is intended for medical professionals (e.g. OT/OTA, PT/PTA, Physicians, etc.) directly related to the rehabilitation of a patient or client. To participate in this CEU and receive credit, the participant must be a licensed, treating clinician. Completion of this course will reward the participant with .1 CEUs or 1 contact hour, following completion of the presentation and a ≥80% score on the quiz. You will have 90 days to complete this course.
Free Online CEU Electrical Stimulation Course for OT’s
NeuroRehab Team
Monday, December 26th, 2022
Course Title:
Electrical Stimulation for Stroke Recovery. A review of evidence-based clinical considerations.
Overview:
This AOTA approved online self-study continuing education class will introduce you to evidence-based practice surrounding electrical stimulation to the stroke population.
The online class is intended for medical professionals (e.g. OT/OTA, PT/PTA, Physicians, etc.) directly related to the rehabilitation of a patient or client. To participate in this CEU and receive credit, the participant must be a licensed, treating clinician. Completion of this course will reward the participant with .1 CEUs or 1 contact hour, following completion of the presentation and a ≥80% score on the quiz. You will have 90 days to complete this course.
Stop Learned Non-Use to Improve Stroke Recovery
NeuroRehab Team
Wednesday, December 21st, 2022
If one asked 10 new stroke survivors the following question, what do you think they would say?
“Would you rather spend most of your time learning compensatory one-handed strategies with your unaffected side, or would you rather focus on improving strength, range of motion and function in your affected limb?” That’s a big question.
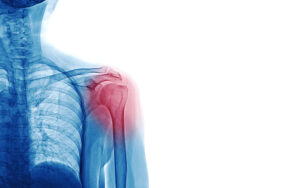
Stroke Shoulder Online CEU Course Now Available
NeuroRehab Team
Thursday, December 8th, 2022
Stroke Shoulder Simplified.
Demystifying subluxation, pain and stiffness.
Robotic Therapy for Stroke. Is it Overrated?
NeuroRehab Team
Friday, December 2nd, 2022
Robot-assisted therapy has become increasingly popular over the last 2 decades. In fact, it is so well-known that out of the 1,300 RCT’s in UE stroke recovery, robotic research leads the pack with 112 RCT’s! There is no doubt robotic therapy, in some form or fashion, is here to stay, however is it a MUST-HAVE or a NICE-TO-HAVE intervention?
Online Shoulder Stroke/Neuro Occupational Therapy CEUs
NeuroRehab Team
Saturday, November 26th, 2022
Shoulder pain resulting from stroke hemiplegia is a common clinical consequence. Hemiplegic shoulder pain can occur as early as two weeks post-stroke but an onset of two to three months is more typical. Frozen shoulder, pain and weakness can negatively affect rehabilitation outcomes as good shoulder function is a prerequisite for successful transfers, maintaining balance, effective hand function, and performing ADL’s activities of daily living.
Should You Strengthen a Spastic Muscle?
NeuroRehab Team
Wednesday, November 23rd, 2022
Great question. The answer is ABSOLUTELY!
For some clinicians, strengthening a hyperactive or spastic muscle is a very controversial topic. The thought of having stroke survivors squeeze their spastic finger flexors or flex their overactive biceps causes some clinicians to cringe.
How to Select a Top OT Stroke CEU – Continuing Education Class
NeuroRehab Team
Saturday, November 19th, 2022

Stroke recovery is a hard and long journey for most patients. There are therapists that “treat neuro patients” and then there are “neuro therapists”. In order for a patient to reach maximum potential with their rehab journey, they will need a clinician that understands, appreciates and knows the neurorecovery process.
Stroke Plateaus are Not Permanent
NeuroRehab Team
Friday, November 18th, 2022
Hand Function SplintsNeuroplasticity
There is no expiration date on neuroplasticity.
Just like athletes and musicians, many stroke survivors will have periodic and temporary plateaus or setbacks as they continue to improve. It is a back-and-forth process. Improve a little, then a plateau occurs. Modify the training and improve some more. Then, here comes another plateau. Modify again. You get the idea.
Occupational Therapy – OT CEUs
NeuroRehab Team
Wednesday, November 16th, 2022
Occupational Therapy CEUs!
Occupational Therapy (OT) CEU’s are part of the necessary requirements to maintain one’s license. In addition, a clinician may seek out paid or free continuing education classes (CEU) to advance his or her knowledge and skill set.
Improve Results Following Stroke with These Simple Steps.
NeuroRehab Team
Monday, November 14th, 2022
Mental PracticeMirror TherapyNeuroplasticitypriming

Priming the Brain Works.
Better clinical outcomes following stroke are associated with interventions such as cortical priming resulting in increased excitability of the motor cortex (Catano et al).
Priming is a technique used to enhance the brain’s ability to re-balance the 2 hemispheres following a stroke. Priming interventions include invasive and non-invasive techniques and can be administered prior to or during therapy.
The Best Way to Treat Shoulder Subluxation
NeuroRehab Team
Friday, November 4th, 2022
Electrical Stimulationshouldersubluxation

The shoulder is the most complicated joint in the human body. It’s also one of the most difficult aspects of recovery for hemiplegic stroke survivors.
Why?
Be Like Mike. Mental Practice Improves Stroke Arm and Hand Weakness.
NeuroRehab Team
Friday, October 28th, 2022
Mental PracticeNeuroplasticity

Be Like Mike.
Before each race, Michael Phelps, the 28-time Olympic medalist, would sit quietly and perform mental reps, imagining his performance step-by-step.
Stroke Survivors Should Look in the Mirror – Daily.
NeuroRehab Team
Friday, October 14th, 2022

Stroke survivors are beautiful and handsome heroes. But it’s not about vanity – it’s about recovery. Mirror Therapy (MT) is a critical intervention – yet vastly underutilized.
Neuroplasticity Following Stroke: How the Brain Improves.
NeuroRehab Team
Friday, October 7th, 2022

The Brain is Fascinating!
The brain consists of 100 billion neurons and 200 trillion synapses. It’s nearly impossible to grasp the complexity and power of this amazing organ. During a stroke, 32,000 neurons die every SECOND, totaling around 1.2 billion for the entire event. That’s a lot, but consider the total neurons in the brain, it’s around 1%. That means 99% of the brain is still intact!
Prevent Falls After Stroke
NeuroRehab Team
Sunday, August 22nd, 2021

Falls can happen anytime and anywhere to people of any age. However, as people get older, or suffer neurological injuries such as stroke, the number of falls and the severity of injury resulting from falls increases. Taking precautions to prevent falling after stroke can help save a life. Falling is the leading cause of accidental home deaths, and they are a major reason for 40% of admissions to nursing homes.
Constraint-Induced Movement Therapy (CIMT) for Stroke Therapy
NeuroRehab Team
Saturday, June 26th, 2021
Constraint-Induced Movement Therapy (CIMT) is a form of treatment designed to decrease the impact of a stroke on the upper-limb (UL) function of some stroke survivors. It is a behavioral approach to neurorehabilitation[2] based on “Learned- Nonuse”.
NIH Stroke Scale: What is it and how does it work?
NeuroRehab Team
Friday, January 22nd, 2021
National Institutes of Health Stroke Scale (NIHSS) is a clinical tool that measures stroke-related neurologic deficits. This measure can be quantified. NIHSS is used in modern neurology for three main objectives;
- to evaluate the violence of stroke to its patients and document the neurological status of the patients.
- To determine the treatment to be administered to patients by planning the appropriate patient care and act as a common language for the exchange of information understood by healthcare providers.
- To predict the outcome of the patient from the illness, both long and short term outcomes. It can also indicate a lesion size and be a measure of stroke severity.
Stroke Survival Statistics: Key Facts To Know
NeuroRehab Team
Wednesday, December 23rd, 2020
Stroke Statistics
Stroke is among the leading causes of severe long-term disabilities. It reduces mobility in more than 50% of its patients who are aged 65 and above. According to NINDS, 15-30% of patients develop a permanent physical disability while most patients regain their hands and legs’ functionality. Symptoms associated with stroke vary from dizziness, fatigue, blurred vision, slurred speech, fatigue, and numbness. However, according to a survey done, only 38% of the respondents knew the stroke’s significant symptoms. The most recognized sign by 98% of the respondents was numbness on one side. Knowing these symptoms is crucial because it can reduce disability in patients. Those who start receiving treatment three hours after the first symptom show less disability than those who receive delayed care.
How Many Repetitions are Needed for Stroke Recovery?
Lynette Diaz, COTA/L
Tuesday, June 9th, 2020
How many repetitions does it take to create changes in the brain? How many repetitions must one complete before movement is strong, volitional and functional? Research indicates the number is high and the answer is more complex than we may think. Factors to be considered are, quality of repetitions, attention during repetitions, number of joints involved in movement, area of injury in the brain to name a few. It would stand to reason the more complex a movement is the more repetitions would be required.
Rewiring the Brain Through Gratitude
Lynette Diaz, COTA/L
Monday, June 8th, 2020

Attitude of Gratitude.
After experiencing a traumatic injury such as a stroke, it may be hard for many people to perceive daily things in a positive light. After all, life is not what it was before. Many stroke survivors go from an independent lifestyle to depending on a loved one. It is evident to see how there is not much room for positive thought.
What You Need to Know About the Stroke Recovery Timeline
NeuroRehab Team
Wednesday, February 19th, 2020
Arm and HandContracture SplintElectrical StimulationHand Function SplintsMental PracticeMirror TherapyNeuroplasticityStretchingSubluxation Slings

You are eager to return to your normal life, so you are ready to learn more about the typical timeline for recovery after a stroke. Keep reading to get some answers to common questions:
- Am I going to get better after my stroke?
- How long is rehab after a stroke going to take?
- What can I do to help my stroke recovery?
Walking and Stroke Recovery: What You Need to Know
NeuroRehab Team
Saturday, January 25th, 2020
Electrical StimulationFoot Drop BraceLegMobilityNeuroplasticity

A stroke can impact any number of life skills. But the ability to walk can be one of the most significant. Many people identify walking as an important goal after they experience a stroke. This makes sense because walking is related to so many daily routines. Every stroke survivor is different. Some stroke survivors might need help to walk a few feet. Other individuals might recover significantly and be able to walk long distances. This article will provide post-stroke walking education for a range of skill levels.
Easy Hand Exercises to Boost Recovery from a Stroke
NeuroRehab Team
Tuesday, January 14th, 2020
Exercise AidsFine Motor CoordinationStrengthening

Launching a hand exercise program begins with understanding how a stroke that happens in your brain can cause problems with your hand. A stroke is basically an injury to the brain due to limited blood flow. The symptoms in the body reflect the area of injury in the brain. So a stroke survivor with hand issues, experienced an injury to the area of the brain that controls the hand.
Improving Sleep Apnea Helps With Stroke Recovery
NeuroRehab Team
Thursday, December 26th, 2019
Sleep Apnea is a known risk factor for stroke and new research suggests that curbing the condition might also aid the recovery of people who’ve suffered a stroke or mini-stroke. New research shows that, among stroke patients, “treatment of sleep apnea with CPAP therapy provides significant benefits, even greater than the benefits of tPA, the FDA-approved drug treatment for stroke,” said study lead researcher Dr. Dawn Bravata.
10 Must-Read Stroke Recovery Books
NeuroRehab Team
Wednesday, December 25th, 2019
When suffering from a brain injury such as stroke, a sense of hopelessness, frustration and vulnerability can occur. Don’t be alone on your journey to recovery! Below are excellent books that provide immense insight into stroke recovery. Click on any of the links for more information.
Adaptive Clothing Tips for Stroke Survivors
NeuroRehab Team
Monday, December 23rd, 2019
Getting oneself dressed is a critical part of being a fully independent person. For a person who has had a stroke, getting dressed can help feel more normal again. This can really help to boost both mood and self esteem.
The tips below will help both the stroke patient and the caregiver make dressing an easier part of the daily routine:
Are You Overstretching Your Spastic Muscles?
Lynette Diaz, COTA/L
Monday, December 23rd, 2019

Stretching can be a very important part of recovery especially following a stroke, when feeling, sensation and movement are returning to a previously flaccid limb. However, is it possible to stretch too much or too hard? Yes it is.
Clinicians frequently see patients handle their affected limbs rather aggressively in an effort to “make it move” or “get it loose”, often stretching their fingers, wrist, elbows and shoulders too far too fast. This may partly be due to lack of sensation or awareness.
Stroke Home Therapy Products Available on Amazon
NeuroRehab Team
Saturday, December 21st, 2019
Stroke survivors often struggle to regain full use of their affected side. Below are a just a few of the available products on Amazon that can help with improving more recovery at home. Whether you are hoping to improve your arm and hand strength or looking for better results with your walking and endurance, the good news is that you can find excellent products for very low prices. Just take a look below and click for more information.
8 Helpful Adaptive Stroke Equipment Ideas To Improve Independence
NeuroRehab Team
Thursday, December 19th, 2019
Adaptive equipment helps stroke patients experience greater independence with everyday life skills or activities of daily living. There is a plethora of assistive devices for all areas of self care including dressing, bathing, grooming, cooking, feeding, toileting, and mobility aids.
Improve Balance With These 5 Affordable Therapy Products
NeuroRehab Team
Tuesday, December 10th, 2019
Decreased balance is a common area affected by stroke. Many patients are prone to falling which could lead to serious injuries. Studies have shown that stroke survivors are twice as likely to fall following a stroke and more than three times as likely as the general population to fall multiple times. About 40 percent of stroke survivors have serious falls within a year of their stroke.
Muscle Tone Following Stroke
Dorothee Zuleger, MOT, OTR/L, DRS
Thursday, November 21st, 2019

Following a stroke, abnormal muscle tone is a common complication. A single muscle or a muscle group may become completely paralyzed. This is known as hypotonic or flaccid or a muscle may increase in muscle tone. This is known as hypertonic or spastic. This abnormal tone usually occurs in the side of the body opposite to the side of the brain lesion.
Returning Home Following a Stroke: Helpful Tips for Modifying Your Kitchen.
NeuroRehab Team
Saturday, November 2nd, 2019

When a stroke patient returns home, the home environment can impact a person’s recovery. The home includes the social and cultural environment such as the people who live there, as well as the physical aspects of the home such as steps and layout. It is important that the home environment be one that supports continuing recovery and safety for the patient. This article is intended to provide basic information to stroke survivors and their families about potential problems with the physical aspects of the kitchen.
Top Ankle and Foot Stretching Products To Improve Flexibility Following Stroke
NeuroRehab Team
Friday, October 25th, 2019

Stroke can cause muscle weakness and tightness along one side of the body. Muscle weakness affects how well you move your body. Without continuous movement daily, your muscles, joints and ligaments will become gradually stiff eventually leading to a contracture.
Search Contracture Foot and Ankle Splints
The ankle and foot is one of the common areas affected by stroke. Often times, foot drop occurs which causes the foot not to clear and lift when walking, which could lead to a risk of falls. When suffering from foot drop, you may experience ankle stiffness over time.
How to Find the Best Stroke Rehabilitation Robot?
NeuroRehab Team
Wednesday, October 9th, 2019

Individuals suffering from neurological injuries, such as brain injury or stroke, typically develop many side effects including, but not limited to, physical weakness, decreased sensation, cognitive and speech impairments and balance just to name a few. Over the past 2 decades, neurological rehabilitation strategies have shifted more from theory-based treatment to evidence-based (science driven) treatment.
How Important is Getting Good Sleep Following Stroke?
Lynette Diaz, COTA/L
Friday, October 4th, 2019

Sleep is an extremely important component to achieve optimal brain health and function. Poor sleep has been implicated in affecting heart function, blood sugar regulation and cognitive decline. Good sleep and normal sleep-wake cycles have been linked to improved cognitive recovery following neurologic insult to the brain such as in the case of both traumatic and non-traumatic brain injury, stroke, multiple sclerosis and parkinson’s. Typically after a neurological insult the normal sleep-wake cycle is disrupted, with the brain injured patient sleeping throughout the night and day with intermittent periods of wakefulness.
Understanding Stroke Exercise Treatment and Technology
NeuroRehab Team
Friday, August 16th, 2019
While in therapy, it is not uncommon for patients and family members to enhance their rehab vocabulary from daily conversations with the clinical team. From the early moments of their arrival, they are immediately bombarded with clinical “whatchamacallits” from physicians, nurses, and therapists. Although the learning curve can be quite challenging, for many it is achievable thanks to Google and Yahoo.
Unfortunately, once the clinical jargon is finally mastered, the patients are preparing for their discharge date that is typically around the corner. It is not until their discharge week that they begin to have serious discussions with their occupational and physical therapists about what exercises to do at home and various equipment that might be needed.
Don’t Be Stuck With the Wrong Stroke Therapist. 7 Must-Ask Questions When Interviewing.
NeuroRehab Team
Tuesday, August 13th, 2019

Suffering a stroke is a life-changing event. The statistics show that many patients will struggle from long-term impairments well after discharge from the hospital. In addition, a majority of stroke survivors will require ongoing rehabilitation on an outpatient basis so continued progress can be made.
As if learning to adjust to a new life following an injury is not difficult enough, finding a good therapist can be challenging. Like every profession, some individuals are hard working, passionate and extremely knowledgeable about their respective industry, while others seem to live day-to-day in an alternate universe lacking basic skills, motivation and common sense. When your recovery is in the hands of a therapist, it is absolutely critical that you identify the best possible clinician that checks all of your boxes so maximum progress can be made.
Mobility and Leg Recovery Following Stroke and Other Neurological Injuries
NeuroRehab Team
Friday, August 2nd, 2019
BiofeedbackBody Weight SupportContracture SplintElectrical StimulationExercise AidsFoot Drop BraceLegLeg BikeMobilityNeuroplasticityRoboticsVirtual Reality
![]()
One of the most common impairments resulting from stroke is paralysis, which can affect a portion or the entire side of the body. Problems with body posture, walking, and balance can be significant. Two thirds of the patients are unable to walk without assistance in the first week after stroke (Jorgensen HS et al. Arch Phys Med Rehabil, 1995). Approximately 35% of survivors with initial paralysis of the leg do not regain useful walking function (Hendricks HT et al. Arch Phys Med Rehabil, 2002). Although 65% to 85% of stroke survivors learn to walk independently by 6 months post stroke, gait abnormalities and poor endurance persists through the chronic stages of the condition (Wade DT et al. Scand J Rehabil Med, 1987).
The Use of Aquatic Therapy as a Stroke Treatment
Dorothee Zuleger, MOT, OTR/L, DRS
Monday, January 28th, 2019
Aquatic TherapyNeuroplasticity

What is Aquatic Therapy?
Aquatic therapy is a type of therapy that takes place in a pool or other aquatic environment. It is a physical and medical rehabilitation specialty that requires the supervision of a trained professional.
Causes and Treatment for Dystonia
Dorothee Zuleger, MOT, OTR/L, DRS
Friday, August 3rd, 2018

What is dystonia?
Dystonia is a type of movement disorder in which muscles in the body contract involuntarily often causing twisting or repetitive movements. Dystonia can range from affecting one part of the body, known as focal dystonia, or can affect multiple/all parts of the body, known as general dystonia. Muscle spasms due to dystonia can be anywhere from mild to severe, impacting daily functioning. Unfortunately, there is no known cure for dystonia, but different medications can alleviate symptoms.
Pain After Stroke
Dorothee Zuleger, MOT, OTR/L, DRS
Monday, May 21st, 2018
Central Pain Syndrome (CPS) is a dysfunction of the pain-conducting pathways of the central nervous system (CNS). The CNS includes the brain, brain stem, and spinal cord. CPS occurs when there is damage to an area of the brain that carries lots of sensory pathways.
People often experience CPS as the result of a stroke, traumatic brain injury, multiple sclerosis, Parkinson’s disease, or spinal cord injury. CPS is commonly referred to as neuropathic pain or sometimes as thalamic pain syndrome by medical professionals.
Left Side Neglect Following Stroke – There is more to the picture
Dorothee Zuleger, MOT, OTR/L, DRS
Thursday, April 26th, 2018
CognitionNeuroplasticitysensory stimulationVisionVisual Aids
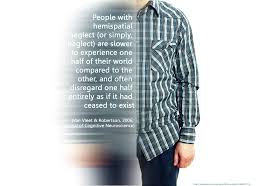
Damage to one side of the brain can cause a lack of attention to the opposite side. Most common is an inattention or neglect to the left side of the body after an injury to the right side of the brain due to stroke or traumatic brain injury. The brain attends to the right side with both hemispheres but attends to the left side with only the right hemisphere.
Recent Study Highlights the Importance of Electrical Stimulation for Spasticity Treatment Following Stroke
NeuroRehab Team
Saturday, April 21st, 2018
BiofeedbackElectrical StimulationElectrode Placement

A recent randomized trial by Yuzer et al., in the Journal of Stroke and Cerebrovascular Diseases 2017, investigated the effects of functional electrical stimulation of the wrist and finger extensor muscles of patients with chronic stroke who had spasticity of their wrist flexors.
Transcranial Magnetic Stimulation (TMS) May Help Stroke Survivors Improve Recovery
NeuroRehab Team
Tuesday, March 27th, 2018
Electrical StimulationNeuroplasticity
Anyone who’s done physical or occupational therapy knows how hard it is not to cheat. The body wants to get back to work, and the easiest way to do that is to use the uninjured limbs to help out. The therapist is there to make sure it’s the injured limb that’s doing the work.