Effect of a task-oriented rehabilitation program on upper extremity recovery following motor stroke: The ICARE randomized clinical trial.
NeuroRehab Team
Friday, October 11th, 2019

Winstein CJ, Wolf SL, Dromerick AW, et al. JAMA 2016;315(6):571-581.
This clinical trial recruited 361 participants, approximately 45 days post-stroke with mild to moderate impairments, for upper extremity retraining in order to improve functional use of the impaired upper extremity. Participants received either a new problem solving approach, Accelerated Skill Acquisition Program (ASAP) for 30, 1 hour sessions, Dose Equivalent Usual Customary Care (DEUCC), or Usual and Customary Care which varied from 0-46 hours. Findings demonstrated that all three groups improved in function (Wolf Motor Function Test) and quality of life (Stroke Impact Scale).
How to Find the Best Stroke Rehabilitation Robot?
NeuroRehab Team
Wednesday, October 9th, 2019

Individuals suffering from neurological injuries, such as brain injury or stroke, typically develop many side effects including, but not limited to, physical weakness, decreased sensation, cognitive and speech impairments and balance just to name a few. Over the past 2 decades, neurological rehabilitation strategies have shifted more from theory-based treatment to evidence-based (science driven) treatment.
How Important is Getting Good Sleep Following Stroke?
Lynette Diaz, COTA/L
Friday, October 4th, 2019

Sleep is an extremely important component to achieve optimal brain health and function. Poor sleep has been implicated in affecting heart function, blood sugar regulation and cognitive decline. Good sleep and normal sleep-wake cycles have been linked to improved cognitive recovery following neurologic insult to the brain such as in the case of both traumatic and non-traumatic brain injury, stroke, multiple sclerosis and parkinson’s. Typically after a neurological insult the normal sleep-wake cycle is disrupted, with the brain injured patient sleeping throughout the night and day with intermittent periods of wakefulness.
Help Quahana Achieve Her Stroke Recovery Fundraising Goals
NeuroRehab Team
Friday, September 20th, 2019

“Quahana ran that way!” is the statement my mother normally heard when she went to round up my sisters and me after Sunday worship services. The Roadrunner was not just a cartoon in my house; it was my life. Laughing, smiling, painting and running was my DNA. Fast forward many years to a warm day in July when I’d just returned from a trip to London for an art conference and I collapsed on my living room floor as I was lacing up my sneakers for you guessed it; a morning run and workout. A carotid artery in my neck; a young woman who had never had a major medical issue; spontaneously dissected (i.e. tore) and subsequently a stroke resulted (with a 10% survival rate!). What followed was weeks in a rehabilitation hospital where I was treated by some of the top specialists and therapists in the country and the world. But what they all shared in common was a clinical belief that stroke recovery typically halts after three years. However, what I know to be true is that I’ve made more recovery after year three than I ever have BUT there is more recovery to be made.
NeuroRehab Directory Launches New Crowdfunding Platform Providing Neurological Patients Access to Life-Changing Treatment
NeuroRehab Team
Wednesday, August 21st, 2019

Fundraising Website Makes It Easy for Patients to Identify Breakthrough Treatment Solutions and Raise Funds to Improve Their Recovery.
Salia Rehab, provider of the world’s largest neurorehabilitation product directory, www.neurorehabdirectory.com, today announced the launch of a game-changing crowdfunding platform that increases treatment access to thousands of patients worldwide.
FundMyTherapy, an innovative crowdfunding platform, helps patients suffering from neurological injuries, such as stroke and brain injury, identify and select therapeutic products that match their needs using advanced sorting features such as impairment, product category, price, body part and/or reviews. Once users find appropriate products and create their wishlists, the proprietary platform enables them to build and personalize fundraising campaign pages to share with family and friends.
Understanding Stroke Exercise Treatment and Technology
NeuroRehab Team
Friday, August 16th, 2019
While in therapy, it is not uncommon for patients and family members to enhance their rehab vocabulary from daily conversations with the clinical team. From the early moments of their arrival, they are immediately bombarded with clinical “whatchamacallits” from physicians, nurses, and therapists. Although the learning curve can be quite challenging, for many it is achievable thanks to Google and Yahoo.
Unfortunately, once the clinical jargon is finally mastered, the patients are preparing for their discharge date that is typically around the corner. It is not until their discharge week that they begin to have serious discussions with their occupational and physical therapists about what exercises to do at home and various equipment that might be needed.
Don’t Be Stuck With the Wrong Stroke Therapist. 7 Must-Ask Questions When Interviewing.
NeuroRehab Team
Tuesday, August 13th, 2019

Suffering a stroke is a life-changing event. The statistics show that many patients will struggle from long-term impairments well after discharge from the hospital. In addition, a majority of stroke survivors will require ongoing rehabilitation on an outpatient basis so continued progress can be made.
As if learning to adjust to a new life following an injury is not difficult enough, finding a good therapist can be challenging. Like every profession, some individuals are hard working, passionate and extremely knowledgeable about their respective industry, while others seem to live day-to-day in an alternate universe lacking basic skills, motivation and common sense. When your recovery is in the hands of a therapist, it is absolutely critical that you identify the best possible clinician that checks all of your boxes so maximum progress can be made.
Mobility and Leg Recovery Following Stroke and Other Neurological Injuries
NeuroRehab Team
Friday, August 2nd, 2019
BiofeedbackBody Weight SupportContracture SplintElectrical StimulationExercise AidsFoot Drop BraceLegLeg BikeMobilityNeuroplasticityRoboticsVirtual Reality
![]()
One of the most common impairments resulting from stroke is paralysis, which can affect a portion or the entire side of the body. Problems with body posture, walking, and balance can be significant. Two thirds of the patients are unable to walk without assistance in the first week after stroke (Jorgensen HS et al. Arch Phys Med Rehabil, 1995). Approximately 35% of survivors with initial paralysis of the leg do not regain useful walking function (Hendricks HT et al. Arch Phys Med Rehabil, 2002). Although 65% to 85% of stroke survivors learn to walk independently by 6 months post stroke, gait abnormalities and poor endurance persists through the chronic stages of the condition (Wade DT et al. Scand J Rehabil Med, 1987).
The Use of Aquatic Therapy as a Stroke Treatment
Dorothee Zuleger, MOT, OTR/L, DRS
Monday, January 28th, 2019
Aquatic TherapyNeuroplasticity

What is Aquatic Therapy?
Aquatic therapy is a type of therapy that takes place in a pool or other aquatic environment. It is a physical and medical rehabilitation specialty that requires the supervision of a trained professional.
Causes and Treatment for Dystonia
Dorothee Zuleger, MOT, OTR/L, DRS
Friday, August 3rd, 2018

What is dystonia?
Dystonia is a type of movement disorder in which muscles in the body contract involuntarily often causing twisting or repetitive movements. Dystonia can range from affecting one part of the body, known as focal dystonia, or can affect multiple/all parts of the body, known as general dystonia. Muscle spasms due to dystonia can be anywhere from mild to severe, impacting daily functioning. Unfortunately, there is no known cure for dystonia, but different medications can alleviate symptoms.
Best Spasticity Treatment Ideas Following Stroke
Dorothee Zuleger, MOT, OTR/L, DRS
Tuesday, July 3rd, 2018

Spasticity is a condition in which a muscle or group of muscles is hyperactive and unable to turn off and relax. After an injury to the brain or nervous system signals to and from a muscle are not regulated as they should be and therefore create abnormal muscle tone. This constant state of contraction can cause, pain, stiffness and shortening of soft tissue limiting normal range of the joint. The degree of spasticity can range from mild muscle stiffness to severe, painful, and uncontrollable muscle spasms.
Pain After Stroke
Dorothee Zuleger, MOT, OTR/L, DRS
Monday, May 21st, 2018
Central Pain Syndrome (CPS) is a dysfunction of the pain-conducting pathways of the central nervous system (CNS). The CNS includes the brain, brain stem, and spinal cord. CPS occurs when there is damage to an area of the brain that carries lots of sensory pathways.
People often experience CPS as the result of a stroke, traumatic brain injury, multiple sclerosis, Parkinson’s disease, or spinal cord injury. CPS is commonly referred to as neuropathic pain or sometimes as thalamic pain syndrome by medical professionals.
Left Side Neglect Following Stroke – There is more to the picture
Dorothee Zuleger, MOT, OTR/L, DRS
Thursday, April 26th, 2018
CognitionNeuroplasticitysensory stimulationVisionVisual Aids
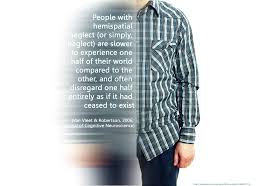
Damage to one side of the brain can cause a lack of attention to the opposite side. Most common is an inattention or neglect to the left side of the body after an injury to the right side of the brain due to stroke or traumatic brain injury. The brain attends to the right side with both hemispheres but attends to the left side with only the right hemisphere.
Recent Study Highlights the Importance of Electrical Stimulation for Spasticity Treatment Following Stroke
NeuroRehab Team
Saturday, April 21st, 2018
BiofeedbackElectrical StimulationElectrode Placement

A recent randomized trial by Yuzer et al., in the Journal of Stroke and Cerebrovascular Diseases 2017, investigated the effects of functional electrical stimulation of the wrist and finger extensor muscles of patients with chronic stroke who had spasticity of their wrist flexors.
Transcranial Magnetic Stimulation (TMS) May Help Stroke Survivors Improve Recovery
NeuroRehab Team
Tuesday, March 27th, 2018
Electrical StimulationNeuroplasticity
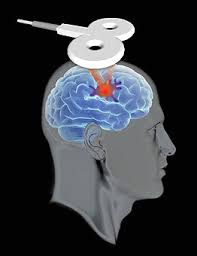
Anyone who’s done physical or occupational therapy knows how hard it is not to cheat. The body wants to get back to work, and the easiest way to do that is to use the uninjured limbs to help out. The therapist is there to make sure it’s the injured limb that’s doing the work.
Intensive Arm Exercises After Stroke Improves Strength and Function
NeuroRehab Team
Wednesday, January 17th, 2018
Arm and HandElectrical StimulationNeuroplasticityOccupational TherapyRobotics
Intensive therapy can help people who have suffered a stroke recover motor function—even if the treatment begins a year or more after the stroke occurred. After a stroke, the brain and body can start recovering immediately and can show improvement up to six months afterward.
Improve Functional Mobility With Lower Extremity Stroke Technology
NeuroRehab Team
Tuesday, December 26th, 2017
BalanceBody Weight SupportElectrical StimulationExercise AidsFoot Drop BraceLegLeg BikeMirror TherapyMobilityNeuroplasticity
One of the most common impairments resulting from stroke is paralysis, which can affect a portion or the entire side of the body. Problems with body posture, walking, and balance can be significant. A patient’s rehabilitation should start as soon as he or she is stable. That could be anywhere from a couple of days to a few weeks or longer. Established guidelines, as well as a huge body of literature, insist that the earlier therapy is initiated the better.
10 Exercise Strengthening Products for Stroke Patients. Improve Arm, Leg, Foot and Mobility.
NeuroRehab Team
Monday, November 20th, 2017
A common impairment following stroke is called hemiparesis or one-sided (“hemi”) weakness (“paresis). Hemiparesis affects about 8 out of 10 stroke survivors, causing weakness or the inability to move one side of the body. One-sided weakness can affect your arms, hands, legs and facial muscles. Individuals with hemiparesis may have trouble performing everyday activities such as eating, dressing, and using the bathroom. Rehabilitation techniques, such as strengthening exercises, can help with speeding up your recovery.
Listed below are 10 exercise products that can help improve your strength following stroke.
10 Must-Try Mirror Therapy Exercises
NeuroRehab Team
Thursday, October 5th, 2017
Electrical StimulationMirror Therapy

The principle of Mirror Therapy is the use of a mirror to create a reflective illusion of an affected limb in order to trick the brain into thinking movement has occurred. Mirror therapy allows the brain to be activated during the imitation movements and interact simultaneously with the motor neurons. For example, if you put your left hand behind a mirror and right hand in front, you can trick your brain into believing that the reflection of your right hand in the mirror is your left. You are now exercising your left hand in the brain!
Stroke Hand Treatment Using Biofeedback Electrical Stimulation
NeuroRehab Team
Monday, September 4th, 2017
Arm and HandBiofeedbackElectrical StimulationHand Function Splints
Activities of Daily Living (ADL) are impacted continuously for may stroke survivors that suffer from limited arm and hand function and movement. Research indicates that Biofeedback and Electrical Stimulation can result in improved mobility and functional use. Biofeedback combined with electrical stimulation (NMES or FES) can be an effective tool in reducing the symptoms of stroke, such as increasing strength and function.
7 Visual Motor Training Devices For Stroke Recovery
NeuroRehab Team
Monday, July 31st, 2017
Following a stroke or other neurological injury, multiple vision disorders can occur including the inability to recognize objects, color vision deficits and difficulty with perceiving various types of motion. Approximately 20% of patients experience permanent visual deficits (Romano JG. J of Neurol Sci. 2008).
According to the National Stroke Association, homonymous hemianopia, which is the loss of one half of the visual field in each eye, is the most common visual disorder. Most people who have vision loss after a stroke do not fully recover their vision. Thankfully, some recovery is possible. Treatment and outcomes will depend on the type of vision impairment and its cause.
Listed below are 7 Visual Motor Training Devices that are currently available on the market that can assist with improving recovery.
5 “Out-of-Shoe” Foot Drop Braces You Should Know About
NeuroRehab Team
Wednesday, July 12th, 2017
Whether you suffered a stroke, living with multiple sclerosis (MS) or experiencing another neurological disorder, experiencing Foot Drop can be quite a struggle. Finding the right support to maintain foot clearance when walking can be challenging at best. Areas of concern include size, comfort, durability and effectiveness.
Listed below are 5 comfortable “out-of-shoe” Foot Drop Braces that are currently available on the market. Although the below braces may be more comfortable to wear, it is important to realize that not everyone will qualify for these lower profile ankle supports. Individuals will need to consult with a healthcare professional to make the most appropriate choice for their needs.
Breast-feeding Mothers at Lower Risk of Heart Disease and Stroke
NeuroRehab Team
Monday, July 3rd, 2017

How to Improve Hand Function Following a Stroke
NeuroRehab Team
Thursday, June 1st, 2017
Arm and HandCIMTHand Function Splints

It is not uncommon for individuals to experience decreased hand function and strength following a neurological injury such as stroke. Sadly, even after 6 months following stroke, over 60% of clients are still struggling to achieve full arm and hand recovery (Kwakkel et al., 2003). Moreover, the inability to actively open the hand for pre-grasp activities is a severe limitation for many stroke survivors. The impaired movements lead to decreased independence in leisure and self-care tasks (activities of daily living). Because this limited function is a difficult challenge, traditionally, clients were required to relearn new compensatory movement patterns and one-handed strategies so functional activities could be achieved.
Intensive 3-Day “Stroke Boot Camp” For Patients Now Available
NeuroRehab Team
Sunday, May 7th, 2017
The Stroke Hand and Upper Limb Clinic, offered by occupational therapists specializing in neurorehabilitation, provides an intensive (3 days, 6 hours per day) upper extremity treatment program for patients suffering from neurological impairments such as spasticity and weakness. The specialized stroke clinic, located in Charleston, SC is geared primarily towards clients that struggle with arm and hand function.
Neuro Rehab Products. What’s right for me?
NeuroRehab Team
Thursday, April 27th, 2017
Arm and HandBalanceCognitionDysphagiaFoot Drop BraceLegNeuroplasticitySubluxation SlingsVision

Listed below are various clinical product categories that you may have learned while in therapy. Feel free to click on any category to see a list of products that may be appropriate for your needs.
Risk for Falls Following Stroke
NeuroRehab Team
Monday, April 24th, 2017

Studies have shown that stroke survivors are twice as likely to fall following a stroke and more than three times as likely as the general population to fall multiple times. About 40 percent of stroke survivors have serious falls within a year of their stroke.
Stroke/Neuro Products That Improve Strength and Function
NeuroRehab Team
Monday, April 3rd, 2017
Arm and HandCognitionCommunicationFoot Drop BraceLegMobilityNeuroplasticityVision

It is true that recovering from a stroke will be an uphill battle for many, however, it is also accurate that the latest research findings regarding neuro recovery are more promising than ever before. How serious are you with embracing evidence into your practice? As a clinician, are you stuck using numerous theoretical-based treatment concepts that have not scientifically been proven to be effective?
Listed below are some of the common interventions supported by research that have shown positive results. How many of the below techniques are in your current therapy toolbox? If just a few, then why?
Best Electrode Position and Placement for Leg and Foot Stroke Rehabilitation
NeuroRehab Team
Friday, March 24th, 2017
Electrical StimulationElectrode Placement

Electrical stimulation, also referred to as e-stim, NMES, or FES, can be an effective tool in reducing the symptoms of stroke, such as increasing strength and function. The success of one’s recovery using electrical stimulation will rely heavily on proper electrode placement.
Listed below are some key video examples of lower limb electrode positioning by Axelgaard. Click on the thumbnail below to visit the video link.
Swallowing Exercises for Dysphagia Therapy Following Stroke
NeuroRehab Team
Tuesday, March 14th, 2017

Neurological conditions can cause trouble with swallowing as a result of damage to the brain, spinal cord and nerves. This type of swallowing problem is called dysphagia. The most common conditions associated with dysphagia include stroke, head trauma, multiple sclerosis, cerebral palsy and motor neuron disease, but any neurological disease can cause dysphagia.
Swollen Arm and Hand (Edema) Following Stroke
NeuroRehab Team
Monday, March 6th, 2017

Edema is swelling caused by excess fluid trapped in the body’s tissues. Although edema can affect any part of your body, it’s most commonly noticed in the hands, arms, feet, ankles and legs. Edema occurs from a variety of reasons. For individuals who are inactive, a collection of fluid in the ankles and legs, fingers and hands can be seen. Individuals that are paralyzed after a neurological injury such as stroke, may have fluid collection just on the affected side.
15 Things Caregivers Must Know After A Stroke
NeuroRehab Team
Tuesday, January 31st, 2017

It can be quite challenging caring for someone with a stroke. When a loved one is first hospitalized immediately after a stroke, families usually assist the hospital team with key personal information as well as convey patient care preferences and serve as the connection between the hospital staff and the patient. You suddenly become the patient’s voice and chief advocate.
Stroke Recovery Using Constraint-Induced Movement Therapy (CIMT)
NeuroRehab Team
Monday, January 23rd, 2017
Arm and HandCIMTNeuroplasticity
What is it?
Constraint-induced movement therapy (CI, CIT, or CIMT) is a form of rehabilitation therapy that improves upper extremity function in stroke and other neurological injuries by increasing the use of their affected upper limb. The focus of CIMT is to combine restraint of the unaffected limb and intensive use of the affected limb. Types of restraints include a sling, a splint, a sling combined with a resting hand splint, a half glove, and a mitt. Determination of the type of restraint used for therapy depends on the required level of safety vs. intensity of therapy.
New Online Directory Collects Reviews of Stroke Rehab
NeuroRehab Team
Monday, January 2nd, 2017
![]()
A new, non-biased website dedicated to assisting patients, families and health professionals with identifying appropriate neuro-rehab solutions and resources has recently launched. The directory is specifically designed for individuals with neurological injuries such as stroke, brain injury, cerebral palsy and spinal cord injury.
Top 5 Apps for Hand Recovery Following Stroke
NeuroRehab Team
Wednesday, December 21st, 2016

The latest research shows that the brain is capable of rewiring and adapting after stroke. Therefore, arm and hand recovery is more possible than previously thought. However, in order to improve function in the upper limb, the client must be willing to incorporate the affected side purposefully and repeatedly.
What is Electrical Stimulation? Advances in Stroke Treatment.
NeuroRehab Team
Friday, December 2nd, 2016
BiofeedbackElectrical Stimulation

Electrical stimulation, also referred to as e-stim, NMES, or FES, can be an effective tool in reducing the symptoms of stroke, such as increasing strength and function. The success of one’s recovery using electrical stimulation will rely heavily on proper electrode placement.
Stroke Therapy Products That Help With Recovery
NeuroRehab Team
Friday, November 25th, 2016
Arm and HandCognitionLegVision

Listed below are various clinical product categories that you may have learned while in therapy. Feel free to click on any category to see a list of products that may be appropriate for your needs.
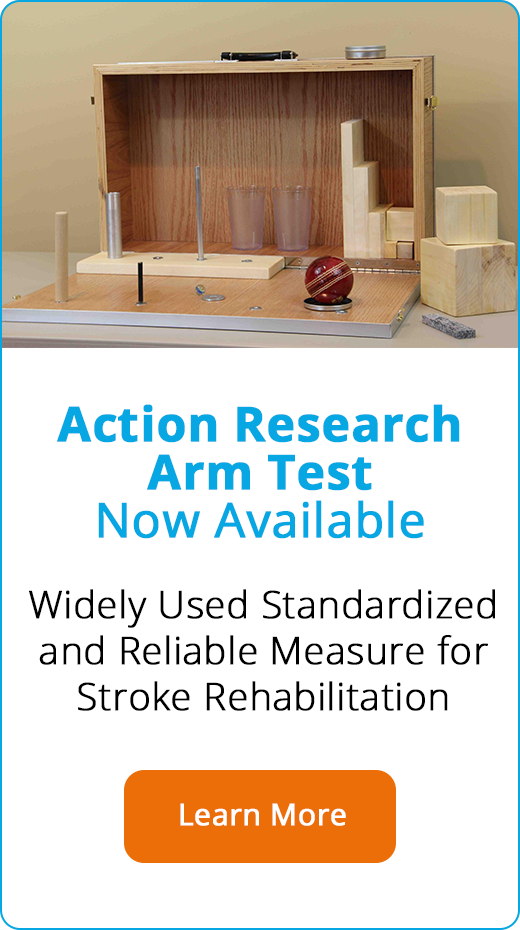
Measuring Arm and Hand Function using the Action Research Arm Test (ARAT)
NeuroRehab Team
Wednesday, November 23rd, 2016

Evaluating the impact of stroke rehabilitation requires the use of reliable, valid, and objective outcome measures. Despite consensus among nationally published guidelines recommending the use of valid and reliable assessment tools, the scientific community lacks direction regarding what outcome measures should be selected for particular evaluative needs. One measure that appears to have general acceptance and embraced by many neurorehabilitation specialists is the Action Research Arm Test (ARAT).
Key Facts About Stroke
NeuroRehab Team
Wednesday, November 23rd, 2016

A stroke, or cerebrovascular accident (CVA), is the rapid loss of brain function(s) due to disturbance in the blood supply to the brain. When you have an ischemic stroke, there is an interruption, or reduction, of the blood supply. Eighty percent of all strokes occur due to ischemia. With a hemorrhagic stroke, there is bleeding in the brain. After about 4 minutes without blood and oxygen, brain cells become damaged and may die. When brain cells are damaged or die, the body parts controlled by those cells cannot function. The loss of function may be mild or severe and temporary or permanent. This depends on where and how much of the brain is damaged and how fast the blood supply can be returned to the affected cells.
Virtual Reality And Gaming Technology Helps Stroke Patients Recover
NeuroRehab Team
Tuesday, November 15th, 2016
NeuroplasticityVirtual Reality

There is strong evidence that repetitive task specific training techniques improve upper extremity function. Task training yields long lasting cortical reorginization specific to the corresponding areas being used. Traditional treatment interventions are based primarily on routine exercises and/or purposeful activities. For many patients, the road to recovery is long and difficult and clinicians are challenged with the daunting task of maintaining patient motivation and compliance while alleviating boredom. Computer based games and virtual reality have recently emerged as novel strategies to maintain motivation and compliance while providing the necessary repetitive training.
New Neuro/Stroke Vision Courses Available
NeuroRehab Team
Monday, November 7th, 2016
![]()
Improve Your Vision Recovery Techniques Now
Approximately 30% of all stroke patients suffer from post-stroke visual impairment (Sand KM. Acta Neurol Scand Suppl. 2013). Following a stroke or other neurological injury, various types of vision deficits can occur including the inability to recognize objects, color vision deficits and difficulty with perceiving various types of motion. Approximately 20% of patients experience permanent visual deficits (Romano JG. J of Neurol Sci. 2008).
New Hand Stimulation Device Now Available for Stroke Survivors
NeuroRehab Team
Wednesday, November 2nd, 2016

A new stimulation device called the SaeboStim Micro is now available for neurological patients limited with arm and hand function. The SaeboStim Micro provides low-level sensory electrical stimulation to the arm and hand using a specialized Electro-Mesh Garment. The unique Electro-Mesh material is not only soft and comfortable to wear at rest, but also during activities. Clients suffering from impaired function, weakness and spasticity can benefit from the much-needed stimulation.
New Stroke App Recommends Evidence-Based Treatment For Arm and Hand Impairment
NeuroRehab Team
Friday, October 21st, 2016
AppsArm and HandNeuroplasticity

It is true that recovering from a stroke will be an uphill battle for many, however, it is also accurate that the latest research findings regarding neuro recovery are more promising than ever before. How serious are you with embracing evidence into your practice?
Wearable Stroke Technology Puts Patient Back in Control
NeuroRehab Team
Tuesday, October 11th, 2016
Arm and HandElectrical Stimulation
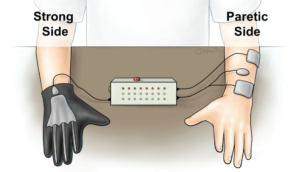
According to new research published in the American Heart Association journal Stroke, researchers at the MetroHealth System, Case Western Reserve University, and the Cleveland Functional Electrical Stimulation Center have developed a glove that allows patients be in control of the stimulation to their weak hand.
Top 7 Stroke Apps for Cognitive Deficits
NeuroRehab Team
Thursday, September 29th, 2016
AppsCognitionmemoryNeuroplasticity

Damage to the brain after a stroke can cause many cognitive changes. Doing things that once were easy may now be hard. Problems with memory and thinking are very common after a stroke and most people will have some difficulties. After a stroke, cognitive rehabilitation can aid the mind just as physical therapy aids the body, according to Psych Central, an online mental health and psychology network. The purpose of cognitive therapy is to improve damaged mental abilities and language skills caused by a stroke.
Where to find Shoulder Subluxation Treatment Options?
NeuroRehab Team
Tuesday, September 20th, 2016
Electrical StimulationshoulderSubluxation Slings

One of the most common areas often affected by a neurological injury is the glenohumeral joint (i.e., shoulder). The shoulder complex is a very sophisticated and complicated joint in the body. It consists of 20 muscles, 3 bones, 3 joints, and 1 articulation. It has the greatest ROM of any joint in the body but at the expense of stability.
Leg and Mobility Neuro Stroke Courses
NeuroRehab Team
Tuesday, September 13th, 2016

Are you caught up with the latest advances in neurorehabilitation? Find relevant stroke neuro courses below to be sure.
Top Stroke Treatment and Technology To Improve Recovery and Function.
NeuroRehab Team
Wednesday, September 7th, 2016
Arm and HandCommunicationLegNeuroplasticityVision
Following an extensive search of 100’s of stroke rehabilitation products and programs, we have summarized the best available products currently on the market for stroke recovery. The products are organized into relevant categories list below. Feel free to click on any category to see a list of products that may be appropriate for your needs.